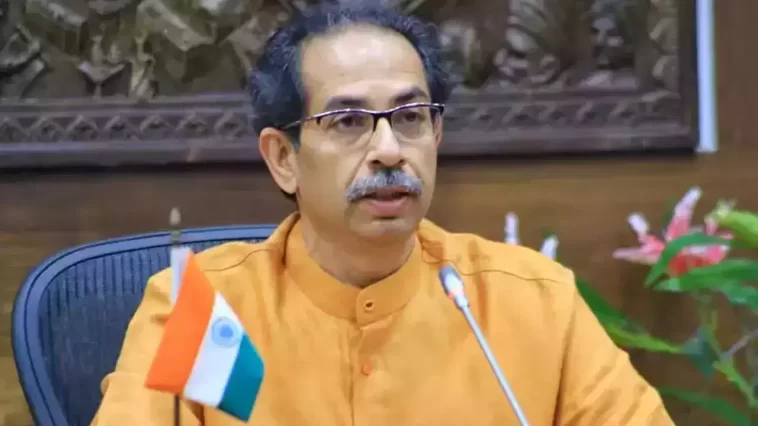
The name Shiv Sena was given by Uddhav’s grandfather, Keshav Thackeray, not the Election Commission, Uddhav stated, adding that the election authority may decide on the poll symbol, but not the name.
Former Maharashtra CM Uddhav Thackeray stated on Monday that he never wanted to be cM, but rather wanted the position for the Shiv Sena, as he had promised to his late father Balasaheb Thackeray.
Uddhav’s tour coincides with an intense political crisis in Maharashtra, as the Nationalist Congress Party has divided between Sharad Pawar and Ajit Pawar, with Ajit Pawar’s faction joining the government. This is the second party separation in the past year, following Eknath Shinde’s rebellion against Uddhav Thackeray and the division of the Shiv Sena.
Monday, Uddhav continued his tirade against the BJP by stating that parties breaking is nothing new, but now they are being hijacked. As Uddhav made this claim against the Election Commission regarding the Shiv Sena name, the Supreme Court agreed on Monday to hear the Uddhav faction’s petition on July 31 — against the EC’s order that the Shiv Sena name and the symbol of the bow and arrow be given to the Eknath Shinde faction.
Also read this:Rajnath Singh Calls Upon Malaysian PM Anwar Ibrahim In Kuala Lumpur
‘How BJP handles new riff-raffs’
As rumors abound that the BJP inducted the Ajit Pawar gang into the government because Shinde and his MLAs will be disqualified, Uddhav stated that if the BJP had maintained its 2019 promise, it would not have needed to carry the carpet for other parties. Uddhav stated on Sunday, “I am waiting to see how the BJP handles the new riff-raffs.” In response to Uddhav’s assertion that Amit Shah guaranteed the BJP and Shiv Sena each 2.5 years as chief minister, Union minister Ramdas Athawale stated that Shiv Sena demanded 2.5 years as chief minister, but Amit Shah never made such a promise.